
What is PRP?
There are 4 main components in your blood:
Serum, Red Blood Cells, White Blood Cells, and Platelets.
When an injury occurs, platelets release growth factors that stimulate regeneration, repair damaged tissues, and reduce inflammation. These processes are essential for maintaining the body’s ability to heal itself.
Platelet-Rich Plasma (PRP) Therapy builds on this natural mechanism. By isolating and concentrating platelets from your own blood, PRP creates a treatment that may promote tissue repair and regeneration.
PRP has been widely used in medical specialties such as orthopedics, dermatology, and sports medicine for decades. It has been used to treat joint injuries, accelerate post-surgical recovery, and even rejuvenate skin in cosmetic procedures like the “vampire facial.” Now, its potential in reproductive medicine is being explored, offering new possibilities for addressing fertility challenges.
How is PRP Made?
PRP is created using a simple and minimally invasive process. A small amount of blood is drawn, much like during a routine medical visit. This sample is then placed into a centrifuge, which spins the blood at high speed to separate its components. The resulting plasma, rich in platelets, is carefully extracted and prepared for use.

Once prepared, the PRP is injected into targeted areas, such as the ovaries or uterine lining, where it may stimulate tissue repair and regeneration. Because PRP is derived from your own blood, there is no risk of allergic reaction or rejection, making it a biocompatible and natural option.
In fertility care, PRP is being studied as a potential way to support ovarian tissue and enhance the uterine lining, offering hope for individuals with diminished ovarian reserve (DOR) or thin endometrial lining.
PRP as a Fertility Treatment
PRP therapy is an experimental treatment aimed at addressing specific fertility challenges. It is currently being studied for its potential to improve ovarian function in individuals with diminished ovarian reserve, enhance the uterine lining’s thickness and receptivity, and increase the likelihood of developing chromosomally normal embryos.
Generation Next Fertility offers two applications of PRP in fertility care: Endometrial PRP and Ovarian PRP.
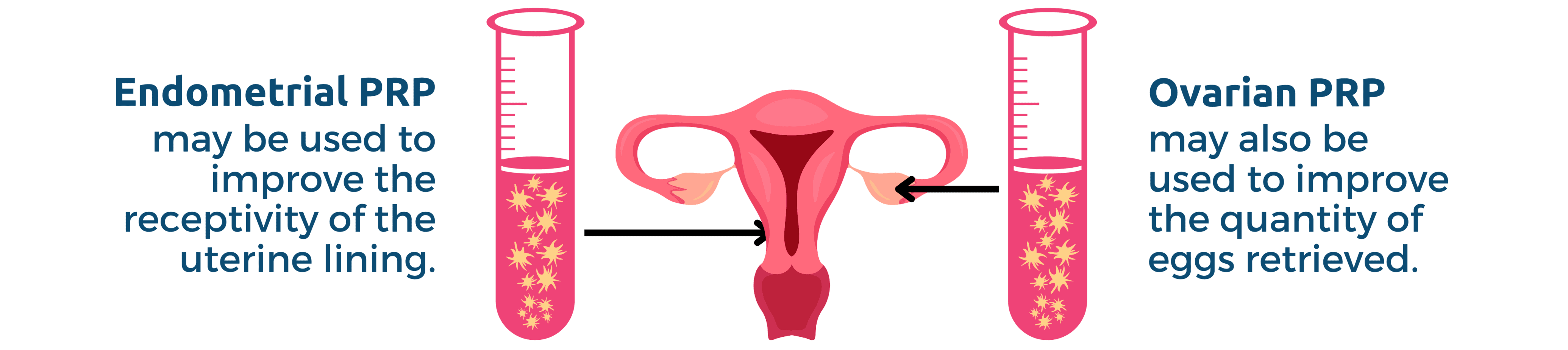
Endometrial PRP
Endometrial PRP is designed to improve the thickness and health of the uterine lining, which is essential for successful embryo implantation. During this procedure, PRP is infused into the uterine cavity using a catheter.
This treatment is generally considered for individuals with a thin uterine lining (often defined as less than 7 mm), recurrent implantation failure, or those preparing for an embryo transfer. In some cases, multiple infusions may be performed within a treatment cycle to encourage better lining development.
Ovarian PRP
Ovarian PRP involves injecting PRP directly into the ovaries under ultrasound guidance. The growth factors in the PRP may stimulate dormant follicles and improve the ovarian environment, potentially leading to better egg quality and quantity.
Ovarian PRP is often explored by patients with diminished ovarian reserve (DOR), poor ovarian response (POR), or advanced maternal age with associated declines in egg quality. The procedure is typically performed one to three months before starting an IVF cycle to allow time for the ovaries to respond.
Ovarian PRP: The Future of Fertility
PRP is increasingly being recognized for its potential to improve the chromosomal normalcy of embryos and optimize fertility outcomes, though its use remains under investigation. To rigorously evaluate PRP’s efficacy, the medical community requires robust clinical trials to confirm its benefits and establish standardized protocols.
That’s why Dr. Jesse Hade and his team at Generation Next Fertility are applying the gold-standard double-blind placebo-controlled study by conducting the world’s first large-scale Ovarian PRP clinical study.


This trial could pave the way for PRP to transition from experimental to a standard of care in reproductive medicine. If successful, the study may make PRP more accessible by opening the door to insurance coverage, benefiting more individuals navigating infertility.
If you’re between the ages of 35 and 42 and have experienced low ovarian response or difficulty with IVF cycles, you may be qualified to participate. By participating, you’ll not only gain access to an innovative treatment but also help advance reproductive medicine through the world’s first placebo-controlled ovarian PRP trial.


